A few days ago I was thinking of the coincidence that the American Civil War had a widely reported military death toll of 620,000 and that is about the same as the death toll from Covid-19 in this country since the pandemic began.
Then magically an article appeared in Time magazine by Rachel Lance, PhD, that summarizes the situation better than I could. I draw pertinent information from her article. (Incidentally, Rachel has written a fascinating book on the Hunley story called, “In the Waves: My Quest to Solve the Mystery of a Civil War Submarine.” I would hope Clive Cussler, who discovered the final resting place of the Hunley, approves. I certainly do. It’s a fascinating story.)
In recent years our civilization has been confronted with a dizzying array of new, or at least newly discovered, diseases Many of these are viral hemorrhagic diseases such as Hanta, Marburg and Ebola. And then there are other viruses such as SARS and its offspring, SARS-CoV-2. And along came ZIKA to join the well known influenza and diarrhea and common cold viruses. Get rid of smallpox and polio and there are always other volunteers to fill their ranks.
And unless we think we are so smart, our old bacterial friends have become antibiotic resistant to keep us humble. That old scourge, Mycobacterium tuberculosis hangs around waiting to catch the unwary. Not wanting to be ignored, fungi are represented by Candida auris along with Cocidioides and Histoplasma. And parasites like the Plasmodium family have never gone away.
So lets compare the Civil War scourges with our current crop.
Here in no particular order are some prominent Civil War diseases (The list is not exhaustive.):
- Typhoid fever
- Typhus
- Malaria
- Yellow fever
- Cholera
- Gas gangrene
- Gonorrhea
- Syphilis
- Diarrhea and Dysentery
- Measles
- Mumps
- Whooping cough (Pertussis)
- Chickenpox
- Pneumonia
- Erysipelas
- Smallpox
It’s worth noting that malnutrition exacerbated the pathogenicity of these bugs. Accounts of the diets of many Civil War soldiers makes one wonder how they were able to function at all. Salt pork? Hardtack? Ugh! And “sanitary” facilities were worse than primitive. A bench across a latrine ditch excavating in one direction with the dirt filling in behind. And handwashing facilities? Are you kidding? It’s no wonder diarrhea and dysentery were rampant. And also why an army on the march was much healthier (think Sherman’s “March to the Sea”).
In spite of vaccines for many of these diseases, especially the childhood diseases, all of these delights are still of current interest.
Here are some current goodies to brighten your day:
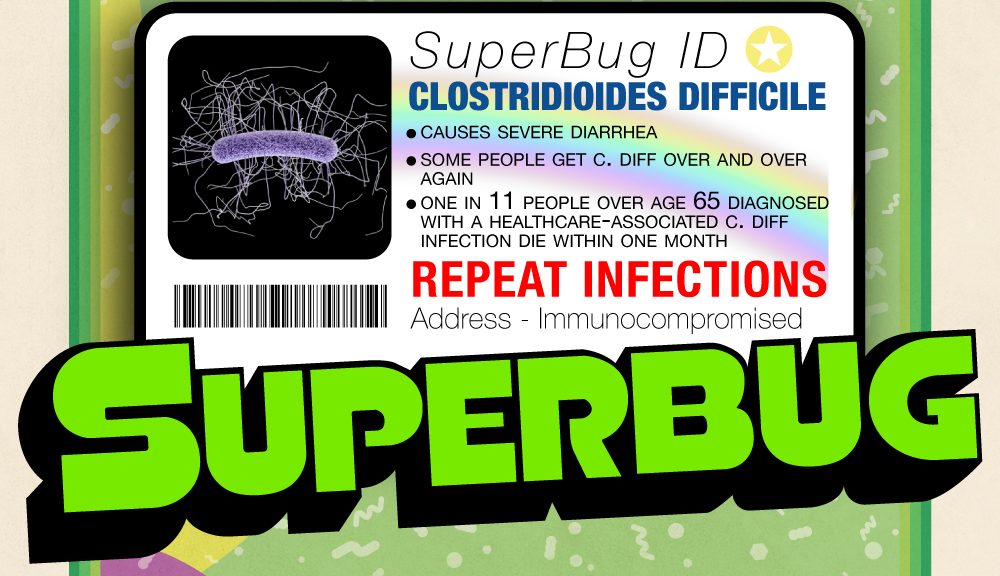
- C difficile (Clostridioides difficile)
- Covid-19 (SARS-CoV-2)
- MRSA (methicillin resistant Staph aureus)
- C auris (Candida auris)
- VRE (Vancomycin resistant enterococci)
- CRE (Carbapenem resistant Enterobacteriaceae)
- Zika virus
- Malaria
- Tuberculosis
- Ebola virus
- Influenza
- Diarrhea
- Pneumonia
- Venereal diseases
- Hanta virus
This, of course, is just a sampling and many more could be listed. But you get the point. While it is still true that most microorganisms are harmless, or even beneficial, there are many that lurk around ready to pounce. If you’re not familiar with it already, you owe it to yourself to look up that old song, “Some little bug is going to find you someday.” (Google it.) The poem dates back to the late 1800s and a number of people have put it to music.
And with that cheery note. . . .
Gordon Short, MD
Brevis Corporation